Bone density measurement
Bone density measurement is an indispensable part of any modern osteoporosis diagnosis, despite the fact that statutory health insurances only cover the costs in exceptional cases. However, it is only to be seen as one component in a larger puzzle and as such only in connection with the respective personal medical history, existing complaints and risk factors.
Since there are now many different methods that measure different things, the experience and “know-how” of the examiner play a decisive role. The quality of piano music also depends primarily on the virtuosity of the pianist. A bone density measurement only ever delivers measured values. However, measured values can not only provide incorrect information, but can also be read incorrectly (just like the notes of a piece of music) – so it depends on the correct interpretation. Today there are a number of different procedures, which, however, measure different aspects of the bone and by no means always actually measure the bone density.
Therefore the informative value of these different methods is not the same or the results with different measurement methods are not at all comparable. Basically, a comparison to assess the course (loss of bone mass or increase in bone density during treatment) is only possible with the same method on the same device and with the same examiner, although some measurement methods do not allow any meaningful comparison at all!
Therefore, before taking a bone density measurement, you should always find out exactly which method is being used, what the informative value of the method is and whether the examiner also has the appropriate experience – especially since you usually cover the costs yourself if you are not privately insured have to.
What actually is bone density?
Density is a physical term and indicates how much mass of any material or object is present in a certain measurement volume. The unit of density is mass per volume – M / V -, e.g. water has a density of 1 kilogram per liter, i.e. exactly 1 kg of water fits into a vessel with a volume of 1 liter. Lead is much denser than water, which is why 1 kg of lead takes up much less space than e.g. 1 kg of springs with a much lower density and correspondingly a much larger space requirement. The density of the bone is somewhere between that of water and lead. With the help of the bone density measurement, the total amount of bone substance present in a certain volume should now be estimated in a very analogous manner, whereby of course only one or two of the total of over 200 bones of the skeleton can be examined as a representative. The higher the density, the more stable the bone should be – at least that’s the theory.
It all depends on the bone structure!
But this is only half the truth. As a liquid, water does not have a fixed structure and is therefore always homogeneous, i.e. if we want to measure the density of water, it does not matter where in a vessel or, for example, where in a lake we do it. Bone, on the other hand, has a highly complex three-dimensional structure in which trabeculae alternate with empty spaces (see illustration). For the measured density, however, it does not matter at all whether there are only a few irregularly arranged thick trabeculae with large gaps in between or many regularly arranged delicate trabeculae with small gaps in between, because the density, by definition, only records the total amount Material in this volume. For the stability of the bone, however, this circumstance is extremely important, just as it is not the weight, but its driving characteristics, workmanship, engine power, safety, etc. that are decisive for the quality of a car. This is why osteoporosis is also defined as a disease that is associated with low bone mass and destruction of the bone structure. New research results increasingly confirm our many years of experience, according to which this destruction of the bone structures resulting from bone breakdown is primarily responsible for the increased fragility of bones in osteoporosis.
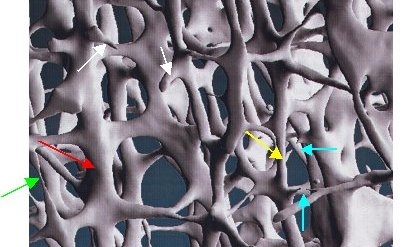
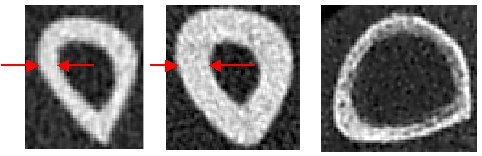
Image: 3-dimensional trabecular structure of the bone. This shows very clearly how the originally very thick trabeculae (red arrow) become thinner (yellow arrow) and finally very thin (green arrow) until they finally break through (turquoise arrows) and at the end have disappeared except for small residual stumps (white arrows). Photo: Scanco Medical AG, Zurich, Switzerland.
The bone density measurement does not detect any structures

Just trying to evaluate the bone on the basis of its density is tantamount to trying to judge the complex architecture of the Eiffel Tower only on the basis of its weight instead of its filigree architecture. The comparison with the Eiffel Tower clearly shows the importance of this highly complicated 3-dimensional arrangement of the struts or the structure that characterizes this construction. It is easy to understand that the rusting through of even a few load-bearing beams could quickly lead to the collapse of the entire structure, even if these missing struts only make up an insignificant part of the total weight. The same applies to the bone, where the measurement of the total amount of bone substance with the help of the bone density measurement only covers one aspect, namely the mass (comparable to the weight of the Eiffel Tower) and not the actual construction. We therefore decided at a very early stage in favor of a measuring method which, in addition to the exact measurement of the bone density, also enables the fine structure of the bone to be assessed.
Which is the best bone density measurement?
The question is asked again and again: which is the best bone density measurement? But this question cannot be answered that way, because first of all it depends on what is actually measured – and there are clear differences between the existing methods. Second, it is crucial why a measurement should be carried out – is it just a rough screening (early detection) or, for example, there is already a justified suspicion of osteoporosis or the measurement even serves to determine the treatment. If you want to cross the Sahara, for example, you will choose a different car than if you are only planning a short jaunt on the beach on vacation or want to transport all your furniture to the new apartment when you move. And third, of course, the examiner’s experience is crucial. To come back to the example of the musician: a good musician will elicit beautiful tones from an inferior instrument, while a bad musician will cause nothing but earache even with the best instrument. The decisive factor is the “know how” and the personal experience and / or his competence.
Methods of measuring bone density
In principle, we have 3 different methods available to us today, with each of these 3 methods in turn having different variants:
US – ultrasound (osteosonography)
DXA – Dual X-Ray Absorptiometry
QCT – computed tomography of the lumbar spine
pQCT – peripheral computed tomography on the forearm (radius)
HRpQCT – high-resolution, imaging, peripheral computed tomography of the forearm (radius) and the lower leg (tibia)
Since each method records very different properties of the bone, the informative value of each method is also different. In the following, the advantages and disadvantages of the individual methods will be discussed. This is not a matter of a rating, as the question of the “best method” also depends on the question at hand, as I said.
In general, it can be said that the measurement of a real (physically meaningful) bone density in mg / cm3 is only possible with computed tomographic methods. The DXA method measures a (physically not sensible) area density in g / cm2. In principle, it is not possible to measure bone density with ultrasound methods! The ultrasonic methods only allow the measurement of a speed of sound with which a statistical risk of bone fractures can be recorded.
Only the high-resolution, imaging, peripheral computed tomography – also used by us – enables, in addition to the exact measurement of the bone density in mg / cm3, the visual representation of the fine bone structure for the first time.
Ultrasound cannot measure bone density
In recent years, so-called “bone density measurements” with ultrasound have increasingly been offered. I deliberately say so-called because, in principle, it is not possible to measure bone density with ultrasound devices.
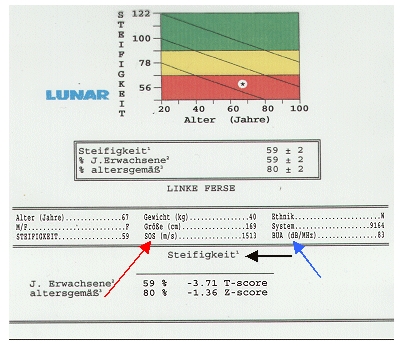
Only the speed of the ultrasound is measured on the way through e.g. fingers, heel or shins, the SOS (speed of sound, red arrow) in meters per second. If you have already had such a measurement carried out on you, you will have seen a colorful display on the printout similar to a traffic light (green, yellow, red) as well as an indication in percent, which is often automatically – but completely wrongly – equated with bone density becomes. A complicated mathematical construct with another measured variable (BUA, Broadband Ultrasound Attenuation, blue arrow) then indicates a so-called stiffness (black arrow). But this has nothing to do with bone density. However, we know from numerous studies that this stiffness correlates very well statistically with the frequency of bone fractures. Although this is important for osteoporosis, the diagnosis of osteoporosis using ultrasound has not yet been possible in principle, regardless of the definition of osteoporosis. If an ultrasound measurement turns out to be bad, strictly speaking an additional measurement of the bone density would be required. But then you could also have the bone density measured right away, at least to save costs!
Ultrasound detects the risk of breakage
Ultrasound is often used in technology for material testing, e.g. to detect fine hairline cracks in oil pipelines. Correspondingly, a kind of bone quality is checked for bones. The speed of the ultrasound is influenced by many factors, including the bone density, the structure of the bone, the soft tissue conditions (muscle mantle, connective tissue, etc.). So far, only a statistical risk of breakage can be determined with ultrasound. Ultrasound does not provide any information about the bone density and therefore neither the extent of a loss of bone mass nor the course during a treatment (increase in bone density?) Can be assessed. Actually, it is still not known exactly which property or quality of the bone is actually recorded with ultrasound. This should be kept in mind when asked to take such a measurement. However, since ultrasound does not have any radiation exposure and the method is also cheap, it should certainly be interesting for the future, e.g. in the sense of screening (routine early detection of an increased risk of osteoporosis). At the moment – and most experts agree on this – the routine use of ultrasound methods in daily practice for diagnosing patients is not yet sufficiently secured!
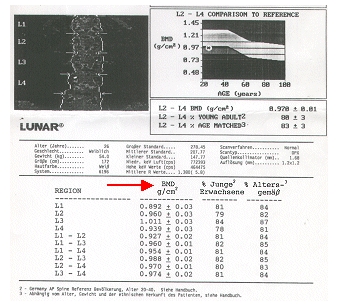
The DXA method (dual X-ray absorptiometry) has been considered the method par excellence for years – hence the name “gold standard”. The measuring points here are the spine and the femoral neck, i.e. the bones where the most dangerous fractures in osteoporosis occur. However, it does not measure a real density, but only a so-called “area density” in grams per square centimeter. However, density has the unit gram per cubic centimeter, i.e. mass per volume. From a physical point of view, a measured surface density makes no real sense, since a surface has no mass by definition, any more than a point or a straight line. Ultimately, the percentage of swallowed (or absorbed) X-rays is measured averaged over a certain area on the way through the body and this value is then converted to a mineral content per area. For this reason, especially in very slim people, bone densities are often determined to be too low, but this is often due to their constitution and not to previous bone resorption.
Slender people usually have thinner bones and the third dimension is not recorded with this method (2-dimensional method). Of course, a tall and very slim person also has a higher risk of bone fractures than a smaller, fat person. However, this has nothing to do with the nature of the bone, but is simply a consequence of the constitution – just as a thin, long branch breaks more easily than a short, thick branch! Furthermore, the DXA method cannot differentiate between the two bone components cancellous and compacta (trabecular bone and cortical bone) (see below) and, in addition, no assessment of the bone structure is possible! Does that still justify the designation “gold standard” today? A hundred years ago, for example, the horse-drawn carriage was still considered the “gold standard” if someone wanted to go on a trip. Today the horse-drawn carriage has largely served its purpose as a means of transport, unless for more romantic reasons at weddings or as a tourist attraction such as in Neuschwanstein. On the image of such a DXA measurement on the spine (lumbar spine) you can see the measurement result in g / cm2 (arrow). BMD = Bone Mineral Densitiy.
Not all bones are created equal
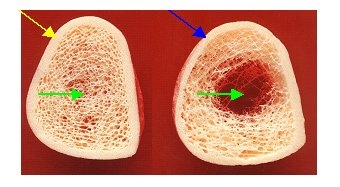
Bones generally consist of two completely different building blocks: a complex 3-dimensional network of trabeculae (comparable to the Eiffel Tower, for example), the so-called trabecular bone, and a compact bone that surrounds it (which surrounds or protects the complex interior like a kind of armor), the so-called cortical bone. You already know the following picture. Here you can see clearly these two bones, the highly complex 3-dimensional trabecular network inside (green arrows) and outside the enveloping compact bones (yellow and blue arrows). In this context, however, the previously mentioned destruction of the trabecular structure is less important than the completely different structure of the two bone components, which also have completely different metabolic behavior and a completely different density. The density of the compact bone is significantly higher (by a factor of 10) than the density of the voluminous trabecular bone, but the compact bone is much slower to remodel than the much more active trabecular bone. The pathologically increased bone loss in osteoporosis therefore almost always affects the trabecular bone and usually much later the compact bone, which only becomes increasingly thinner in advanced osteoporosis (right picture, blue arrow) (yellow arrow left: normally thicker for comparison compact bone).
Since the DXA measurement (as the “gold standard”) cannot differentiate between these two building blocks, if the total bone density measured is low, it does not have to be decided whether a lower bone density is due to a previous bone loss or due to an originally lower build-up, and in particular one less build-up of compact bone is due. Because of the much denser structure, this contributes a significantly higher proportion to the overall density. Tall, slender people in particular often have a lower overall bone density due to the thinner, compact bone (greater length growth at the expense of thickness growth), as the pictures below (taken with our special imaging computer tomography) on the respectively compact bone of the forearm (spoke) clearly show to let.
On the left you see the bone of a 1.82 meter tall and slender woman with relatively thin, compact bone, in the middle you see the same bone in a woman who is only 1.61 meters tall and is much thicker. If only a total bone density is measured, this may be significantly too low for the tall woman (left) due to the thinner, compact bone. With the DXA method, an incipient osteoporosis was actually determined here. However, this was not the case, as no degradation processes were still recognizable and the trabecular bone still had normal bone density and structure. The rather thin, compact bone was therefore normal for the tall patient (top left picture), in stark contrast to the example of another patient (right picture, yellow arrows), in which the compact bone was obviously not just clear after extensive previous degradation processes narrowed, but also appears visibly “perforated”. Of course, this is no longer normal. It is therefore important to determine the density of the two bones separately (if you measure a normal oil level in your car, that does not mean that the petrol tank has to be full too) and it is also important to actually see the bones , because it makes a big difference whether – as in these examples – the compact bone has always been relatively thin due to the constitution, for example, or has only become so thin due to previous bone degradation processes. A low bone density alone is therefore by no means sufficient evidence of the actual presence of osteoporosis.
On the trail of osteoporosis with space technology
We have been using the method of high-resolution, peripheral, quantitative computed tomography – pQCT, since the mid-1990s, which has a number of advantages over the method just described. Not only can we measure the boil densities of the two dissimilar bone components separately, in the form of a real physical density in milligrams per cubic centimeter, but we can also make the fine structure of the bone visible for the first time, which opens up a completely new and previously unknown dimension . This technique was originally developed for studying astronauts when it was discovered that they suffered severe bone loss while staying in weightlessness. The main thing here was to be able to precisely determine the relatively small bone losses due to the rather short stays in space, which also requires a high level of accuracy of the method for control measurements (reproducibility).
The high-resolution, imaging, peripheral computed tomography – pQCT
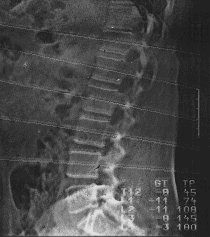
his method used by us combines for the first time all the prerequisites for an accurate and reliable assessment of the bone and the risk of osteoporosis. The measurement locations here are the forearm (spoke, radius), a bone that is not weight-bearing, and the lower leg (shin = tibia), a weight-bearing bone. It cannot measure the bones where the most dangerous osteoporotic fractures occur (vertebrae and femoral neck), but this is more than offset by the many advantages. In addition, we now know that the trabecular bone (trabecular bone) and the compact bone (cortical bone) behave differently, but behave in the same way in the entire skeleton. So if there is increased bone breakdown in one of these two bone components, then this breakdown affects the trabecular bone or the compact bone in the entire skeleton (albeit with certain local differences). Since osteoporosis is by definition a systemic skeletal disease and consequently a disease of all bones, it can in principle also be determined on every bone. The fact that the typical osteoporotic fractures on the forearm, vertebral body or the thigh neck occur more frequently than on other bones is primarily a consequence of the respective accident mechanism, as in a car accident also always the most exposed areas such as fenders Forearm or femoral neck) or the wheel suspension (axle, roughly comparable to a vertebral fracture). However, in some forms of osteoporosis, especially the osteoporosis caused by the consumption of cortisone, the spine seems to be affected by osteoporotic bone loss (stem-dominated osteoporosis), so that in these cases a bone density measurement on the spine is essential (if none gross wear or vertebral fractures are present on the lumbar vertebrae LWK 1 to LWK 4, which are normally measured, which can significantly falsify the measured density values or even render them unusable – X-ray image!).
How high should the bone density be?
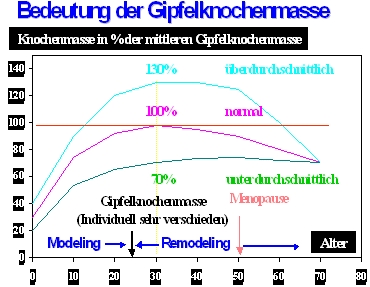
The bone density measurement provides us with a measured value to answer the question of how much bone substance is still present. In order to be able to assess this value correctly, we would also have to know how high the bone density should actually be or how high the bone density was originally at the age of about 20 years (at this age you have your peak bone mass or “peak bone” mass “largely built up). Now this value is usually not known – who has had their bone density measured at the age of 20? Therefore, the assessment of the measured bone density is always only a statistical one, i.e. the measured value found is based on a statistical average value of the bone density that has been previously determined for each method in many healthy younger women or men. This “peak-bone-mass” or summit bone mass – as well as, for example, body size or weight – is of course very individual and by no means the same for everyone!
The importance of summit bone mass
However, this is very important for the assessment or assessment of the measured value, as the following figure should clarify. If, for example, at the age of 70 the measurement of the bone density shows a value of 70%, this does not mean that the bone density is 70% of the starting value – i.e. the original peak bone mass – but 70% of the average peak bone mass of younger women or men. This can mean that the original summit bone mass has actually been 100% (or more) of this average value and 30% of the originally existing bone mass (or more) has already been lost. However, it can also be the case that the originally existing peak bone mass has never been more than 70% of this average value, because, for example, for hereditary, developmental or constitutional reasons, less bone mass was simply built up at a young age. If there has not yet been a serious loss of bone mass, the bone is still in its “original state”. This clarification is important, because 30% bone loss or more inevitably leads to a destruction of the bone structure and only in this case would the risk of bone fractures be significantly increased in the sense of osteoporosis. It also makes a difference whether I only have 70 of the original 100 euros in my wallet because I forgot 30 euros at home and didn’t even have it with me or because 30 euros were stolen from me!
Only the structure provides information
This essential difference cannot be identified by measuring the bone density alone. This shows the real importance of the bone structure representation. Here is an example:
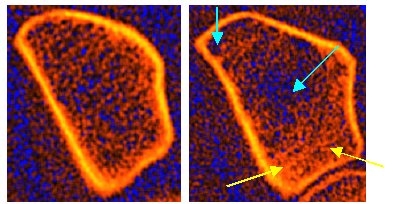
The two pictures show the forearm bone (spoke) of two women. Both had a practically identical trabecular bone density (trabecular bone), on the left it was 71%, on the right 72%, in each case based on the average (trabecular) bone density of younger, healthy women, which in both cases would correspond to osteopenia. On the left the trabeculae appear somewhat loosened, but still largely regular and normal, while on the right a clear breakdown of the trabeculae with already pronounced destruction of the bone structure can be seen (turquoise arrows). In addition, one can see numerous diffuse densities that can be traced back to attempted repair measures (microcallus formation) (yellow arrows) and which make the measured bone density even higher than it actually is.
In the case on the left, it is more likely that the summit bone mass was originally below average, because there are no visible, coarser signs of previous, bony degradation processes. Initially, this patient certainly does not need any treatment, at best calcium and vitamin D as a precaution. In the case on the right, the pronounced structural defects suggest that there have been significant previous osseous degradation processes; in spite of an apparently only moderately reduced bone density, osteoporosis in need of treatment is certainly present here. One can already see from the pictures that there is probably a rapid loss of bone mass (high turnover or fast-loser situation) or at least there was.
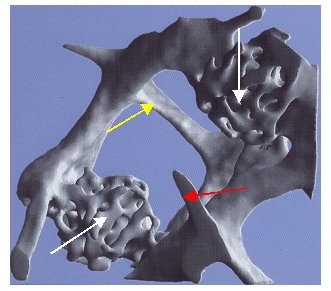
Microcallus formations arise through repair processes in the bone, e.g. if individual delicate trabeculae have broken through, but a connection (bridge formation) occurs again through these repair processes. Here, as is so often the case, nature chooses a path that can be described as trial and error. From the two ends of the broken trabeculae, so to speak, “sprouted” numerous “roots” with the aim of “reunification”. When these sprouts meet again, a new connection is created. However, since numerous attempts have to be made to achieve a successful “reunification”, a kind of conglomerate of connections arises in the event of a “reunification” that has actually been successfully completed, as the illustration on the right clearly shows. The yellow arrow marks a normal connection, the red arrow a residual trabeculae after a so-called microfracture (“small break” of a single trabecular bone) without reunification.
The two white arrows show successful reunions of originally perforated trabeculae after such a microfracture. It is easy to see that these repair processes (micro-callus formation – white arrows) require far more bone material than a normal connection. Therefore, the bone density in an area with several microcallus formations will be significantly higher, which can lead to serious misjudgments of the measured bone density, if such microcallus formations cannot be detected by means of an imaging method (such as the computer tomography we use).
If the city of Paris – to go back to this example – had placed an order to check the stability of the Eiffel Tower, certainly no engineering firm would be entrusted with this very coveted task, which would simply “weigh” this steel colossus. Because every conscientious structural engineer will examine the condition of the struts, i.e. their structural integrity, and the more precise and convincing the method he can use, the sooner he would be awarded the contract. The detection of bone structures is just as important in diagnosing osteoporosis. It is not only important to recognize osteoporotic patients in order to be able to treat them accordingly, but also to avoid unnecessary treatments only because of a possibly reduced bone density!
Computed Tomography of the Spine – QCT
In addition to the computed tomography method we use, there is also a method that uses this technique to measure bone density on the spine. This also measures a real bone density in milligrams per cubic centimeter and it is also possible to determine the bone densities of the two different building blocks – trabecular bones and compact bones – separately, but so far no corresponding representation of the bone structures. In addition, the radiation exposure with this method is significantly higher than with the method we prefer. As a rule, measurements are taken on 2 or 3 lumbar vertebrae and this is also a trabecular-specific procedure (especially so-called postmenopausal osteoporosis is primarily characterized by an initially predominant loss of trabecular bone mass). One of the main problems with QCT is not infrequently the different reference collectives used; the average peak bone mass of Californian women (according to data from the University of San Francisco) is often used as the basis for assessing the measured density values. However, these usually have higher bone densities than Central European women (sun all year round, foods fortified with vitamin D). In addition, the assessment using the so-called T-Score according to the WHO definition of osteoporosis is often used for assessment, which is actually not allowed for this method. In our experience, a disproportionately large number of patients are classified as osteoporotic patients with this method. These partially incorrect assessments are less due to the method than to the lack of knowledge of some users who offer this method (mainly radiologists).
Bone density measurement – when for the first time?
A first bone density measurement around the age of 20 to 25 would be ideal, because then you could record your personal peak bone mass and thus know your own base value, so to speak. So you would later no longer only have to rely on a statistical assessment based on the average peak bone mass, but you could determine exactly whether and, if so, by how much your own bone density had already decreased. Of course, this only applies provided that the control measurement would be carried out with exactly the same device and in the same institute. Normally, a first measurement would make sense for women at the onset of menopause, because from this point on the risk of increased bone mass loss increases significantly. If there are several burdensome risk factors, an earlier point in time might be preferable. In men, the optimal point in time for an initial bone density measurement is mainly dependent on any risk factors that may be present.
Bone Density Measurement – How Often?
This question can certainly not be answered universally. If the first bone density measurement at e.g. 50 years of age turns out to be completely normal or even above average, a control measurement after e.g. 5 years is certainly sufficient. If the result shows a significantly reduced bone density, a control measurement should of course take place earlier, e.g. after 1-2 years. The main purpose of a control measurement is to assess the possible extent of a loss of bone mass. If the bone density is high or the loss of bone mass is low, there is of course only a much lower risk of osteoporosis than if the bone mass is already low and the bone mass loss is high. If osteoporosis already exists and this is also being treated, check-ups are usually necessary annually or at least every 2 years in order to check the success of the treatment and the response to the medication.
The fast and slow loser concept
Depending on the extent of the loss of bone mass, we differentiate between a “high turnover” (rapid bone loss) and a “low turnover” osteoporosis (slow bone loss) or a “fast loser constellation” from a “slow loser constellation”. In this context, “almost loser” means rapid bone loss which, by definition, accounts for more than 3% of the trabecular bone that was originally present (at the time of the first measurement). A “slow-loser constellation” exists if the loss is below 3% per year (also based on the much more active trabecular bone). 3% per year add up to well over 30% bone loss in 10 years (“interest effect”)! The following picture example of one of our patients shows such a pronounced “almost loser constellation” with over 30% (!) Bone loss within only 4 years.
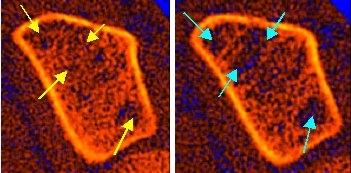
In the picture on the left (basic examination from November 1996) one can see signs of degradation in the area of the trabecular bone (yellow arrows), the bone density was then still within the normal range. However, these incipient structural defects have already raised the suspicion of an increased rate of bone degradation. We therefore suggested the patient to have a check-up after 1 year without any further treatment. After 1 year a pronounced loss of the trabecular bone was found, which amounted to approx. 9% and thus corresponded to a pronounced “almost loser constellation”. Despite this massive bone loss, the patient was unwilling to accept treatment, but nevertheless came regularly for further control measurements once a year. After a total of 4 years, the bone loss in the area of the trabecular bone was already over 30% (!). The picture on the right from November 2000 shows the now large-scale mining zones (turquoise arrows) with a considerable increase in the spotty demineralization areas, which were already visible during the initial examination 4 years ago – but only hinted at at the time. This patient still does not accept any drug treatment for fear of possible side effects, as she is fundamentally against any kind of “chemistry” – not even in view of the increasing risk of a vertebral body rupture. This pronounced bone loss could have been reliably prevented with modern drugs. A diagnosis without consistent treatment is – as you can see here – informative, but obviously of little help. In addition, this example clearly shows the importance of the representation of the bone structure, because despite the originally normal bone density, the previous bone loss was already recognizable on the structural images!
Rate of bone loss – important for treatment
Whether or not there is a rapid loss of bone mass (fast-loser situation) is of course very important for the treatment (therapy). Even with normal or only slightly reduced bone density (osteopenia), treatment should be started in the presence of a high turnover or fast loser situation in order to prevent further bone loss. A stable bone situation – despite the presence of osteopenia or osteoporosis according to the WHO definition, which is only based on the bone density measured using the T-Score system – is, in our opinion, not always in need of treatment (in the sense of drug therapy) . However, in such a case, regular checks should of course take place (the rate of bone breakdown can change again at any time) and appropriate basic measures such as simple calcium / vitamin D prophylaxis and regular exercise (sport, senior sport) should be started. Strictly speaking, if you park your car on a sloping road, you would only need to apply the handbrake if the car rolled down. Nevertheless, as a precaution, you would probably always apply the handbrake prophylactically on such a road!
